Nationwide Medicare scams have taken $100M+ meant for senior's medical bills, investigation reveals
CHICAGO — Scammers have taken more than $100 million meant for senior citizens' Medicare bills, which comes from taxpayer money. The swindlers were only caught after making $3 billion worth of fake Medicare claims.
One tiny office in northwest suburban Roselle that's consistently submitted less than $8 million in Medicare claims a year charged more than $260 million to the government in only a few months.
That amount was in large part earmarked for urinary catheters, even though none of the products listed on Whaba Medical's windows — like oxygen, walkers, scooters, and wheelchairs— are used to go to the bathroom.
"These people should be in jail," said one Google review, with another exclaiming, "What horrible people." The words "catheter" and "fraud" popped up repeatedly in reviews.
"I noticed a cop was patrolling our little parking lot here, which is unusual," said Robert Perez, a neighboring business owner.
Perez said CBS News Chicago was not the only one sniffing around in the normally quiet office park off Lake Street.
"I saw what I believed to be the feds, but who knows what they were?" Perez said. "They were all wearing suits carrying out like all their files."
Even though a call to Whaba Medical didn't go through, CBS News Chicago eventually got a hold of a man listed on years worth of state records for the equipment provider. He said he sold Whaba Medical in December 2023. The prior owner said mail forwarded to him in January 2024 showed some "strange" billing activity by the new buyer.
He suspected fraud and reported it to Medicare. That led to handing over information to the FBI, which apparently began looking into the small Illinois company as part of a massive nationwide investigation.
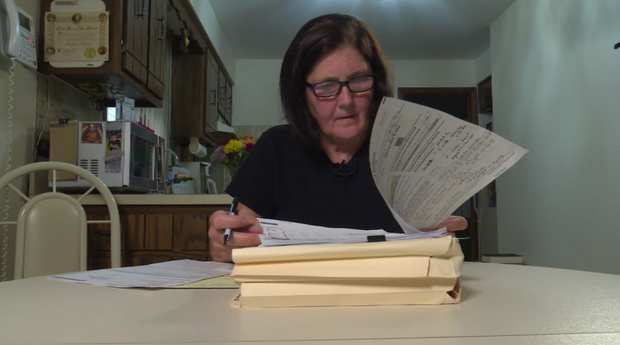
"Just this alone is so frustrating to me, that they missed this," said Ann Caruso, a Medicare fraud victim.
About 30 miles away in Bridgeport, a simmering Caruso shuffled through months of research about her Medicare account. More than $15,000 was billed in her name, and a little over $12,000 of it used taxpayer dollars that fund Medicare. Another $3,100 came out of her supplemental insurance.
"I said, 'Can you put a note in my file saying that this charge was not my charge?'" she said. "I never ordered catheters. I don't use catheters."
$3.8 billion in fake claims
It's not just happening to her. The scam has hit people in Hawaii, Ohio, and Texas, like Tom England. CBS News Texas traced Konaniah Medical, the company that charged more than $8,000 in catheters to England's Medicare account to an empty office. CBS New York also found crickets at G&I Ortho Supply in Brooklyn.
It was the same story in the Chicago area where nobody was home back at Whaba Medical either.
But these companies claimed to be very busy in 2023 and earlier this year. They charged Medicare a combined $904 million in catheters, according to the National Association of Accountable Care Organizations. The nonprofit's research found exponential increases in catheter billings by nine other companies, too.
Altogether, it amounted to nearly $3.8 billion in fake claims on real people's Medicare accounts.
"What else is out there that we're missing or they're missing?" Caruso said. "We're not talking like $300,000. Three billion dollars. That's taxpayer money."
Medicare was careful to say that this was not $3 billion wasted. A spokesperson said its system stopped 95% of payments on the phony claims.
In a statement, a spokesperson for the Centers for Medicare & Medicaid Services (CMS) said, "It is important to note that just because something is marked "payable" does not mean funds will be paid – that is not the final step in the process. If a provider or supplier is under investigation and their payments are suspended, that information is not reflected on a Medicare Summary Notice (MSN) for people with Medicare. That is, it may appear as though CMS has paid for an item or service, when in fact, we have withheld payment while we investigate."
Still, a lot of damage was done.
"I think it's crazy"
Pamela Ludwig owns Pretty in Pink Boutique, a legitimate business. It was not the "Pretty in Pink" that charged catheters to the Medicare accounts of Caruso and many others.
"We were getting hung up on, yelled at," Ludwig said.
Ludwig's Tennesee-based shop sells mastectomy supplies. Her staff got bombarded with angry calls anyway, all saying her business billed their insurance for urinary catheters.
"We were getting hung up on, yelled at," Ludwig said.
In an online disclaimer, Ludwig wrote, "We are not the company that billed you." She said she was forced to put the disclaimer on her website because of the mistaken accusations.
"We're in business to do good for the community, not to harm anyone," she said. "And Medicare fraud only harms all of us."
In an April Congressional hearing, federal watchdogs from the Government Accountability Office sounded the alarm about improper payments by Medicare, again. The GAO reports detailed how Medicare can better prevent fraud and protect precious tax dollars.
Leslie Gordon helped write the recommendations as the GAO's Medicare director.
"They need to make sure they're doing the fingerprint-based criminal background checks to ensure the identity of those providers," Gordon said.
It's unclear if stronger vetting would've stopped whatever happened at Whaba Medical. The Illinois Attorney General's Office is now investigating the case as well.
"Obviously, I think it's crazy," Perez said. "I find it weird that it could be happening in such a small little, unassuming area."
In a statement, the Centers for Medicare & Medicaid Services (CMS) said, "CMS is committed to preventing fraud and protecting people with Medicare from falling victim to fraud. To that end, we can take swift actions to prevent illegitimate payments from going to bad actors when we have credible allegations of fraud. CMS does not confirm or discuss the existence of any ongoing investigation to ensure we do not compromise the integrity of the investigative process. However, that does not mean that CMS is not taking actions behind the scenes."
The spokesperson said the agency has worked with the U.S. Department of Health and Human Services Office of Inspector General and the Department of Justice to investigate health care fraud schemes and referred cases to law enforcement as appropriate.
The Roselle office is now on the radar in one of the biggest fraud investigations in U.S. government history.
"So 11 or 12 companies were able to do this and Medicare couldn't catch it?" Caruso said. "That's scary."
Caruso worries the $3,000 in fake claims charged to her supplemental insurance, Blue Cross Blue Shield Illinois, will impact her premium. CBS News Chicago asked the provider multiple times if that was a legitimate concern, but the company did not respond.
If a person with Medicare receives items or services they did not order or authorize, or if they notice their Medicare Summary Notice (MSN) includes items or services they did not order or receive, they should immediately contact 1-800-MEDICARE (1-800-633-4227) to report the situation. People with Medicare can also call their local Senior Medicare Patrol (SMP).
To find the SMP in their state, they can go to the SMP Locator or call the nationwide toll-free number 877-808-2468 and ask for the SMP phone number in their state. People with Medicare coverage can request a new Medicare number if they suspect their current one has been compromised.